Bonassar Group helps develop new cell therapy
By Tom Fleischman
When a regenerative medicine company in New England looked to expand its knowledge base a few years ago, a member of its management team did what most of us would when we’re looking for answers: He searched the internet.
It didn’t take long for Stephen Kennedy, chief technology officer at Waltham, Massachusetts-based Histogenics, to come across the name of Larry Bonassar, the Daljit S. and Elaine Sarkaria Professor of Biomedical Engineering.
“I’d been doing some research on leaders in tissue engineering,” Kennedy said. “Obviously, Dr. Bonassar’s name came up very quickly, so I went through his website and contacted him.”
That led to some “interesting conversations,” Kennedy said, and eventually a sponsored research agreement (SRA) with the Bonassar Group, which focuses on the regeneration and analysis of musculoskeletal tissues, including bone and cartilage. One of Histogenics’ main products is NeoCart – a cell therapy that uses a patient’s cells grown in a collagen scaffold to repair knee cartilage defects.
NeoCart is in the final phase of a U.S. clinical trial, with top-line data expected in the third quarter of 2018, and got a huge international boost recently, thanks in part to the Bonassar Group’s help with development and testing.
On Dec. 21, Histogenics announced an $87 million licensing agreement with biomedical technology firm Medinet to develop and distribute NeoCart in Japan. Bonassar and Kennedy said Cornell-based efforts played a significant role in the deal.
“We think we have contributed to their having a really much more in-depth understanding of how their product works,” Bonassar said of Histogenics. “And I think that has been integral in their ability to, in this case, talk to the regulatory agencies in Japan as well as potential commercial partners there.”
Kennedy concurs.
“We really didn’t have a clear picture of the various biomechanical properties of the tissue,” he said. “Once we did this work and compared it to what we see with native cartilage, it really elucidated that. The overall benefit [of the collaboration with Bonassar] is that we’ve really been able to clearly identify the mechanism of action of NeoCart.”
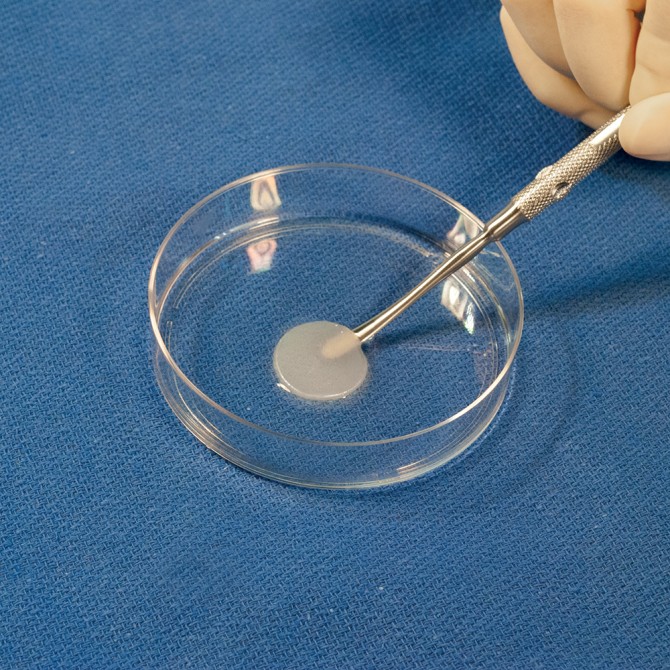
NeoCart is produced by harvesting cartilage cells from the non-weight-bearing cartilage surface of the patient’s femur. The cells are expanded, embedded in a collagen scaffold and then incubated using a proprietary processor.
The scaffold is porous – “think of it almost as a sponge, where the holes are mostly aligned,” Bonassar said. One of the challenges for Histogenics was determining just how stiff the cartilage implant had to be to handle the wear and tear inside a knee joint.
“You can say, ‘It needs to be exactly what the native tissue is,’ but we know that’s not true,” said Bonassar, a faculty member in biomedical engineering and mechanical and aerospace engineering. “But given that, how do we identify a threshold? How do you know when it’s ready?”
Through some novel testing methods, the Bonassar Group identified a mechanical transition point that occurs during the cell-culturing process. Gradually, the cells fill in the “sponge holes” of the scaffold so that it goes from porous to solid, Bonassar said.
“What happens when you take something with a bunch of holes in it and squeeze it? Those pores basically buckle,” he said. “But if you fill in the holes, eventually you’ll reinforce those pores so they don’t buckle. And we’ve been able to directly evaluate this process and demonstrate that if the pores are sufficiently full, you’ve reinforced the whole scaffold and it behaves differently.”
Of course, everyone is different – all the way down to the cellular level. That makes each implant unique, Bonassar said.
“You can say, ‘I’m going to put in half a million cells on this scaffold,’ but a half million cells from a 19-year-old and a half million cells from a 58-year-old might behave very differently.”
Histogenics’ SRA with the Bonassar Group runs through 2019. Future goals include streamlining NeoCart’s manufacturing process using 3-D printing technology. Kennedy said he was originally drawn to Bonassar’s lab because of its work in bioprinting: “That was actually the original aim of the SRA, and it evolved from there and the biomechanical testing sort of took over.”
Another objective is to devise a way to test the product during production, possibly through spectroscopy and composition analysis. Currently, multiple units have to be made in order to test them, which drives up cost and production time.
“We’re working with them quite actively now to see whether we can help them redesign their bioreactors to be able to take measurements in a way that won’t disturb the samples and won’t require that they sacrifice them before they put them in patients,” Bonassar said. “We’ve got some ideas. Clearly, we don’t have all of the answers yet, but that’s part of the fun.”
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe